Yes, I’ve been very quiet. VERY quiet. I know, I’m sorry. Recovery from my November surgery took quite a lot of effort. On top of that, the mobility restrictions meant my psoriatic arthritis decided to complain, so I was fighting on two battle fronts.
My ankle surgery took place on November 28, 2023. My first completely pain/discomfort free walk was March 22, 2024. 16 weeks and 2 days.
I’m not repeating the details previously documented, so if you are catching up, read the surgery article linked above first! The moon boot was better than the cast and knee scooter for sure. I could shower without “bagging” my leg in plastic bags! I didn’t have to sleep in the moon boot! I was no longer doing three-point turns in my small apartment or constantly reversing in and out of spaces. I could drive! I was no longer so totally dependent on other people, I had a modicum of freedom.
I was allowed to go to the gym to do upper body work. ONLY upper body work, but at least it was something! The gym staff looked at me a little askance, but let me in.
I was to gradually increase the percentage of weight on that leg each week and could try proper shoes at week four of moon boot life. I will admit I snuck into shoes a couple of days early because the moon boot meant my legs weren’t the same length and my right piriformis muscle was not overly impressed with that situation. I was VERY careful though.
At my 12 week post-op my surgeon was very happy with how everything had knitted and I was finally allowed to go to the physiotherapist. It is amazing how weak your calf and ankle muscles can become after 12 weeks of no use. Surprisingly, this physiotherapist wasn’t as bossy as the knee physiotherapists: exercises every second day instead of every day.
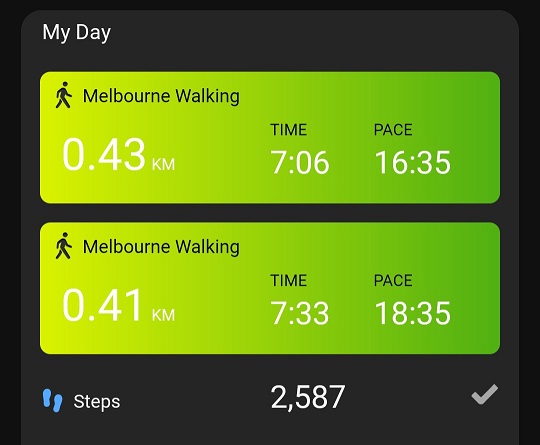
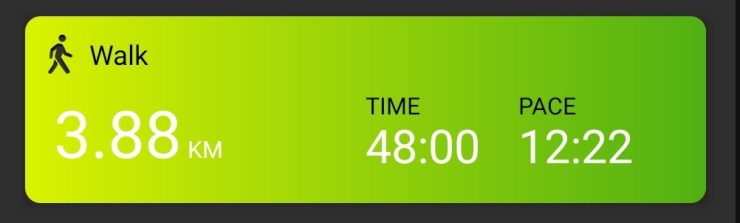
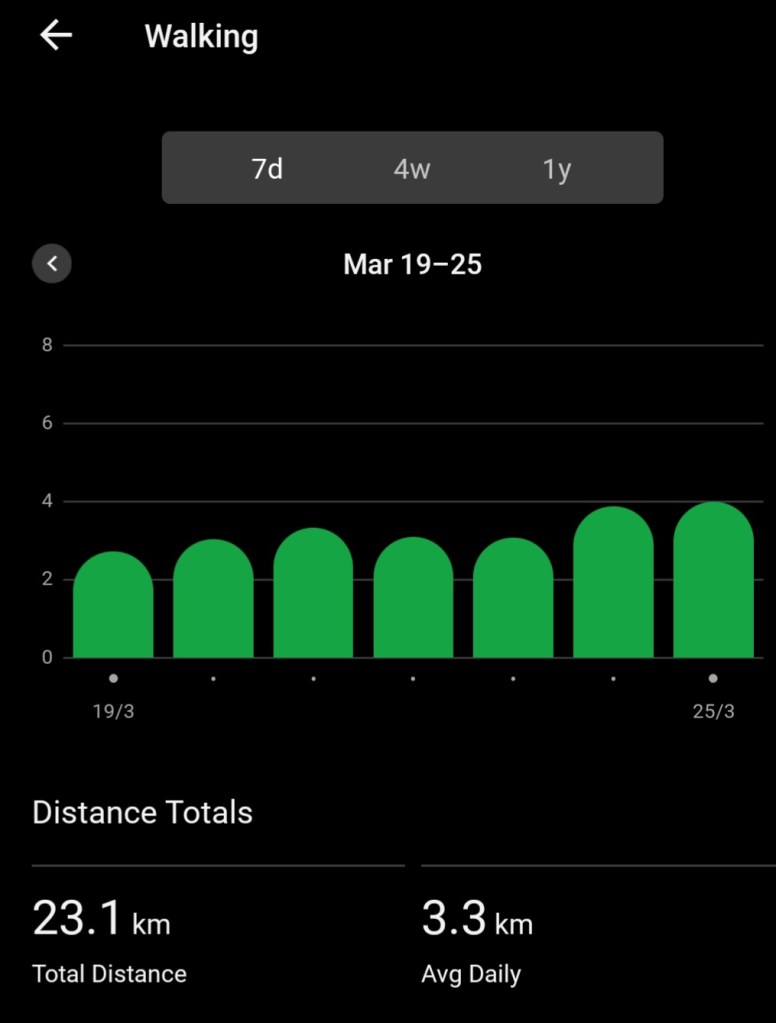
On February 14 I started short walks – between 500 and 800 metres depending on how the ankle was feeling. I managed my first 1 km walk on February 20 and have slowly built up from there. March 21 I walked 2 km in one hit! I should add I was doing multiple walks a day by this stage, with the physio’s permission.
While the ankle/foot wasn’t really painful, it wasn’t 100% comfortable either until March 22. That was the day I felt free!
Funny conversation with surgeon at the 12 week post-op.
Me: “So I have no restrictions now?”
Surgeon: “No, you’re fine!”
M: “So I can do the leg press?”
S: “Sure!”
M: “So what weight can I start at?” (Thinking to myself 50 kgs seemed reasonable to start)
S: “Oh, just the plate, no weights!”
M: Thinking – that sounds like a restriction to me!
It always pays to clarify. I think maybe he didn’t consider his nearly 70 year-old patient was going to be doing things like the leg press. Have I got news for him!
I have interesting rehabilitation exercises, such as standing on one leg for 30 seconds and calf raises on one leg. Now, to be honest, I still cannot do the one-legged calf raise, but I’m getting there with a little help from the other leg. A little less help each day. Hoping I can do the single leg calf raise by my next physio visit!
So yes, it was well worth it, but man alive, am I glad I only have two ankles. I’ve learnt a lot of this experience and will plan the next one with the knowledge I now have about how VERY different this is from knee replacement surgery.
Of course not every ankle surgery will be exactly the same as mine. Other patients may spend less time in a cast for example. Or more time in a moon boot. It definitely isn’t as easy as knee replacement though.
Due to the lack of exercise during those weeks of recovery, my back is not happy. It is getting happier now I am back to a more normal routine, but some days have been quite tough. Moving is not as bad, most of the time, as being stationary, luckily. My back has been under control for some years, due to the work I keep doing on my posterior chain to support it, but at my age we decondition faster than in our twenties – I’m having to build up that strength again. The shoulders and wrists didn’t like the crutches either – the psoriatic arthritis complained. Both wrists and shoulders are now improving with increased exercise and no irritation from the load of crutches.
One thing I wasn’t happy about was once I could walk 1 km, I discovered I’d lost another point on my VO2 Max reading. I was devastated. While I don’t do high intensity exercise and therefore don’t expect a high VO2 Max reading, I do want something healthier than “poor”! Thankfully, I’ve worked hard enough this week (shown below) and last week to recover that measly one point. The lost of the one point had worried me because it was the continuation of a downward trend that started early 2023 and so desperately want to turn it around and get back to where I was.

So that’s it for this ankle. When the next one will be done is debatable. Naturally the surgeon looks at risk mitigation from the perspective of the risks of surgery. I’m looking at it from the recovery perspective. It doesn’t matter how brilliant his surgery is if I am not well enough to manage the recovery properly and at this point in time I’m still not sure we will get my psoriatic arthritis under control. I needed my wrists, shoulders, piriformis and back to be better behaved. I managed, but it was tough.
Onwards and upwards! I need another 3,700 steps today to hit my daily goal, so off I go!