It goes like this. On April 6, 2024 I started my NINTH psoriatic arthritis medication. Sequential, not together! Some medications have a loading dose period: this is one of them. So for four weeks I have injections once a week. Then I move to monthly injections. The first monthly injections are the week after the last loading dose injections, so effectively the patients have weekly injections for five weeks in a row.
You’ll notice I said injectionS – no, that is not a typo. The dose is not available in Australia in one pen, so I have to use two pens. This is not a problem for me as I find the pens really easy to use.
A previous biologic I was on was fine during the loading phase, then when I got to the normal doses, in that case an injection every eight weeks, I found it wasn’t as effective. I’d be great for about three weeks, then steadily feel worse for the next five weeks. Not a great situation to be in.
So, while I feel very good right now, I am waiting until June/July to see if this medication will be effective for the full four weeks between injections. Of course I am hopeful! But that is why I feel like I am in a holding pattern. There are things I want to do, get involved in, but I feel I can’t yet commit to anything that involves other people until I know how this treatment is going to pan out longer term.
At least I’m not taking any NSAIDs or prednisolone and I’ve taken Panadol Osteo about three times a week. YAY me! Or YAY the new medication. Because I’m not taking those additional medications (and I’m moving), I’m also managing to shed the weight gain that occurred while I was taking them. Thank you, 2023. Not my favourite year, let me tell you.
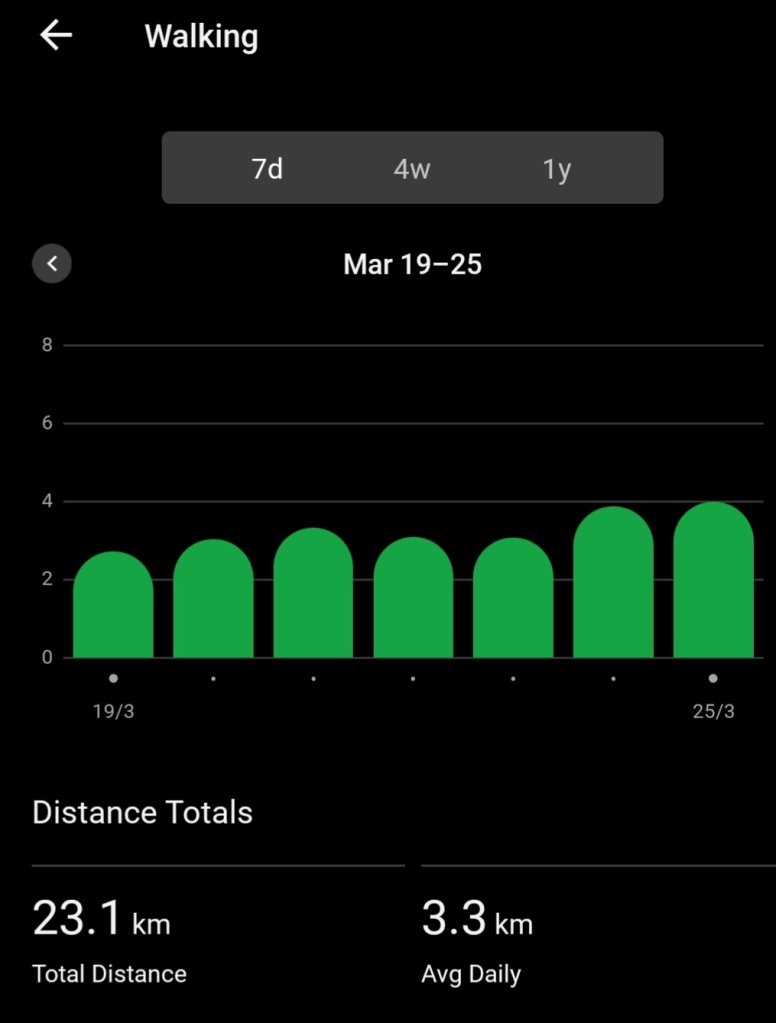
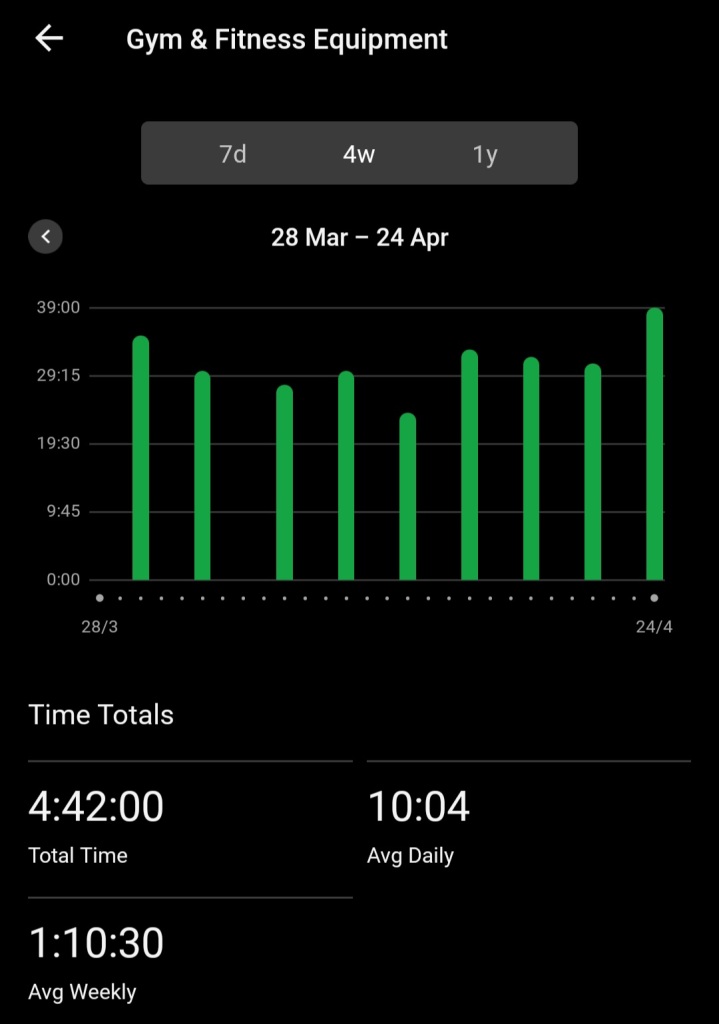
Another aspect of being chronically ill that is driving me nuts at the moment is the amount of effort required to remain, well, functional. So much planning goes into ensuring I get the movement required, balancing with the rest required. Then of course I’ve just had nine months of rehab exercises from first the knee replacement surgery then the ankle surgery. Not to mention the cast and the knee scooter and the moon boot! At the moment I’m kind of on the come back trail: the last four weeks have been good, let’s keep going. My first walk after the ankle surgery was February 14, a whole 0.8 of a kilometre. Now is much better.
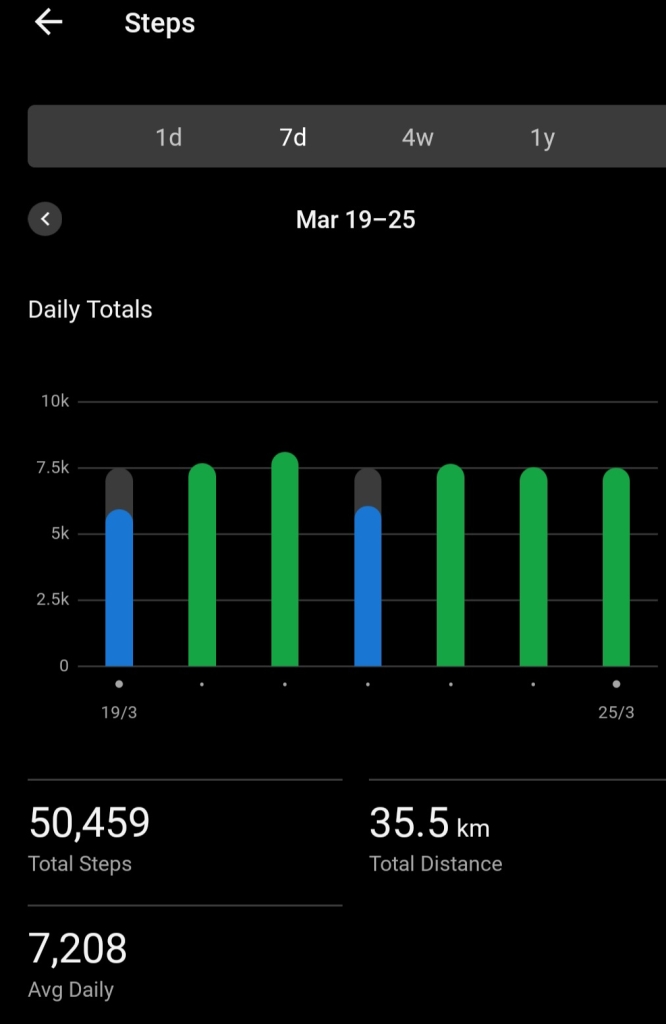
I drop my target step count on the days I lift weights, which is every third day. Some days the weather may impact my step count! This is Melbourne, after all: we can have sunshine one minute and a howling storm five minutes later.

Reconditioning one’s body after nine weeks essentially immobile when that body is already challenged by psoriatic arthritis (and, umm, advancing years) requires a bit more planning that usual. Yesterday was a classic case. I did not make my 7,500 steps. I needed another kilometre, but for whatever reason/(s) a few things were grumpy by the end of the day. I opened my front door. Stood there for about 30 seconds and decided (sensibly) this was not happening. Closed the door and came back inside!
My lower back did play up off and on once I got moving again. Being “misaligned” for nine weeks on the knee scooter then the moon boot was not something my back muscles and left glutes liked AT ALL, I discovered. Lots of heat packs and stretches involved and all is now back to normal.
In summary, some days I end up feeling as if all I do with my life is work at keeping this disease under control. In the early years, I was still working, I had a purpose to keeping it under control. Now there are days when I wonder why on earth am I putting in all this hard work? Which is why I need to be DOING something other than just “keep active”. I need to have something to DO. Which explains the holding pattern dilemma. Thank goodness for my psychologist allowing me to vent!
I’ll get there! It is just a frustrating time and we all have them.
I’m still happy to be past the tip of the bell curve (top photo) for my daily step count given my situation. And remember, that is only Garmin wearers, many of whom will be very active, not the whole population!
By the way, I’m freaked out by the number of people that are freaked out about patients injecting ourselves! Many diabetics have been doing it for years! I’m not sure why we (i.e. those with other conditions) are seen any differently.