If you have not done so already, read Part I before reading this article. Also pay close attention to the caveat therein.
Please bear in mind it is impossible for me to cover everything in one or two articles. My aim is to give you ideas and tips about how to get started.
Choosing Your Trainer
If you have an exercise physiologist – problem solved! They can develop a program for you and will know all the stuff I’m (hopefully) putting in laymen’s terms in this article! But not all of us do have exercise physiologists. Like any profession, you have to find the right one for you. I’m very happy with mine, but I have pointed out to one (in a hospital environment) that what I was being asked to do was not suitable given my overall situation at the time. Communication is, as with so many things, key. Recently I met a personal trainer who has become a osteopath as he wanted to increase his knowledge. This would be another ideal situation, of course!
From here on, I am writing as if you do not have an exercise physiologist.
As I described in Part I, different trainers have different areas of expertise, the same as doctors. No doctor graduates from medical school as a rheumatologist. Fitness coaches/personal trainers don’t finish their certification with a specialist knowledge of chronic illness patients. We need to find a trainer with either further education in this field or considerable experience – or willing/wanting to learn.
What questions should we ask? That is going to vary from person to person, depending on your particular condition/(s) AND the stage of progression of your condition/(s). I can give you some ideas, but you will need to think about your own specific situation and what might be the best questions to ask in your situation. What you are looking for is the trainer’s willingness to and hopefully knowledge about adapting exercises to suit your situation.
One question I would ask is do they recommend the chest press be done with free weights on a bench, or on a chest press machine. Yes, we already know I’d MUCH prefer to be doing the chest press with free weights – but I don’t for safety reasons as explained in Part I. I’d be looking for a trainer who was aware of the risk mitigation.
Another may be simply asking what do they know about your medical condition/(s). Hopefully you know enough to know if their answer is correct! If they don’t, are they willing to research. Effectively, your trainer becomes part of your “treatment team” and while you don’t need another doctor, you need them to understand the basics of things like flares and inflammation.
Side arm raises are an exercise where the angle can be changed from the standard lateral raise. Or the elbow can be bent slightly. These modifications depend on individual circumstances – I adjust my technique, you may not need to. This is a classic example of why the questions you ask need to be tailored to your situation.
The big one is the old “no pain, no gain” mantra. For a healthy person there is some truth to this – you might feel like you’ve lifted weights a day or two after you’ve lifted weights especially if you are lifting to failure. None of us will be doing that! If we feel discomfort doing an exercise it could be for a number of reasons:
- Could be because we haven’t used that muscle or muscle group for a while
- Could be because there is currently some inflammation there
- Could be because over time we have “protected” that area and it has become weaker than it should be
The list is rather endless but we must stick to the pacing principles of Chronic Pain Management – feel a change, stop! NO “pushing through”. As I pointed out above, it may be a solution to change the angle, or drop the kilograms you are lifting, or do less repetitions (or drop kilograms and increase reps – the possibilities are many). The bottom line is you need a trainer who is well aware of these adjustments and who will NOT encourage you to continue at ANY level of discomfort.
Program Options
What sort of program you do will depend on your condition(/s), your background with strength training (if any), your level of overall fitness and your energy levels. While yes, you want to improve, you also have other things to do in your life such as cooking, laundry, driving and you need to ensure you don’t use all your energy on any one activity. Some chronic illnesses impact our energy levels quite severely, others not so much.
Be guided by the trainer – that’s why you are paying them after all – but be guided by yourself. If you feel the program design is too much for you when first starting out (e.g. do you feel wiped out the next day) then cut it back, add exercises back in slowly.
You may start with something like (I just plucked these out of the air for illustrative purposes):
- Warmup
- Leg press
- Chest press
- Seated row
- Leg extension
- Bicep curls
That’s not a heavy load BUT it is enough to see how your body reacts. If you feel fine, add a couple more exercises in.
Remember, the more exercises you do per session, the more careful you may have to be about increasing the weights because more exercises means using more energy. Increasing kilograms means using more energy. You don’t want to use too much energy all in one go. Avoid the Boom/Bust cycle!
Also, see the “How Often” section. You can split the workload!
Starting Kilograms
Recently I took a much younger friend, Tanya, to the gym with me. Tanya had expressed an interest in building her strength but was a bit wary of hitting a gym full of body building champions (my words, not hers). My gym is nothing like that so I invited Tanya along. Essentially she is healthy, not a chronic illness patient. She had recently noticed that physical work had resolved some shoulder pain she had been experiencing and that had driven her to think more strength training would be a good idea.
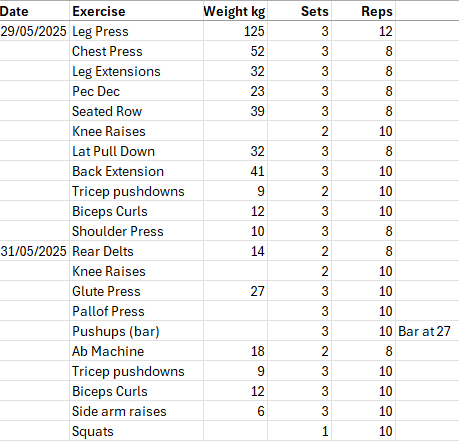
We did a warmup on the treadmills then headed for the leg press. I am mortified by my own (now) measly (by my expectations of myself) 125 kg leg press, and innocent me assumed given Tanya’s relative youth and health status, she’d easily lift that. I was wrong. We needed to drop the kilos. I have lifted weights most of my adult life, I have a history. Tanya doesn’t. So even though I’m sad I can’t lift what I once did, Tanya’s legs had no such experience! On one machine I had to set the weight to no weight at all. I will say Tanya is now more inspired than she already was to build her strength!
And she posted a lovely compliment: “Can this woman lift some serious weight, yes she can! Put me to shame!” I didn’t put her to shame at all really. I suspect it was a simple case of my friend underestimating my abilities due to my age (compared to her age) and medical conditions! Tanya is 16 years younger than I am. I probably overestimated her abilities due to her youth and recent physical work.
The lesson here is your starting weights could be anything. DO NOT STRUGGLE. Yes, you will see healthy people lifting to failure (keep increasing the weight until they literally fail to lift that weight). WE are NOT going to EVER do that, unless you are lucky enough to go into remission!
Start with a weight that feels comfortable for you for that exercise. You might start by doing 8 reps a set instead of 10. Increase the reps each session, then increase the weight and drop back the reps at the new weight. As I mentioned in Part I, I tend to build up to 12 reps a set before I increase the weight. At the new weight I’ll do 8 or 10 reps depending on the exercise.
If your trainer says, “That looks too easy for you, let’s increase”, that’s fine to TRY, but if you feel any discomfort or you struggle, drop back. Pacing rules rule!
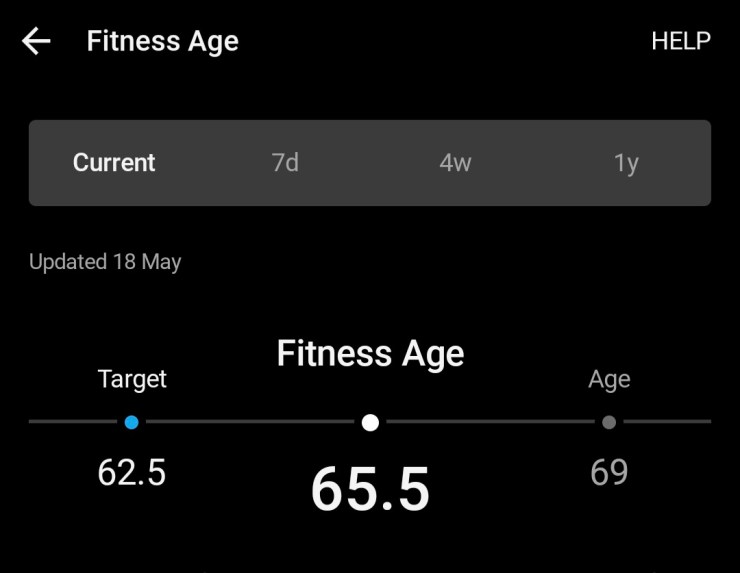
How Often
When I started back I did strength training twice a week. I then increased to every third day. Now I’m doing three times a week and I very much doubt I’ll go beyond that, simply because I want to ensure I don’t overdo it. It also depends on what else you are doing. I walk and swim. You might cycle or run. Some readers will still be working, may have families you are caring for: any number of other aspects of life that require energy. And let’s not forget those darn medical appointments you still have to fit in – they take energy too.
Initially, I dropped my step goal on the days I did weights. I no longer do that, but it is an approach that works in the early days. It is all about balancing your energy use while you build more energy reserves.
Now I’m going to paint a general picture. I’m not saying this next idea is what you should do, I’m saying this is an example of what you MAY do. The trainer and you decide on a program. Be aware it doesn’t have to be done all on the same day. You can split the exercises. Spread the exercises over two days. You may do upper body one day, lower body the next. Or you may find a bit of both is better. For example, my wrists have been problematic from time to time. Most upper body strength training exercises involve use of the wrists in one way or another. Consequently, at those times, I do not do all my upper body on one day. That may aggravate my wrists, not something I’m keen on.
We have to be a bit more flexible (no pun intended) on how we approach strength training, especially in the early stages.
Other Adjustments
I’ve seen stroke survivors in the gym exercising one side of their body. I’ve been there in a moon boot doing upper body only. Other times I’ve done lower body only because my shoulders were flaring. I’ve walked in on crutches and only done upper body. We need to be prepared to be flexible in our approach. Sure, I’m working on increasing my weights, but there’s been days when my body just says, “no, not today” and I have to drop my weight (on whatever exercise) for that specific day.
Don’t get hung up about increasing constantly. That’s not what this is about, we aren’t aiming to compete at the Olympics, we just want to maintain our independence (see the articles at the bottom of Part I).
Don’t feel defeated if today you can’t lift what you lifted three days ago. We have chronic illnesses that often seem to have minds of their own and while we are in charge of managing those conditions, part of managing them is listening to our bodies.
I wear a mask. Yes, I’ve been asked, “Are you going to lift weights in a mask?” Yes, I am. I am immunosuppressed and have underlying inflammatory conditions. I DO NOT need Covid! I am not lifting the sort of kilos that would have me gasping for breath. I will say I can only manage about 500 to 700 metres on the treadmill with a mask, but that’s all I need for warmup.
Protein
Check how much dietary protein you are consuming. Many of us don’t eat enough protein and if we add strength training to our “To Do” list we need to ensure we are getting enough. I am not a nutritionist so I suggest you talk to your GP or a nutritionist. I have cited this article before, specifically related to inflammatory diseases (and inactivity).
Effects of inflammation and/or inactivity on the need for dietary protein – PubMed
I found this interesting as I realised at one point my protein intake was not reaching even the recommended levels for a healthy person AND my pain had increased. I asked a physiotherapist was he aware of any research re pain and lack of protein. He wasn’t. I discovered I felt better when I upped my protein intake. I then went searching for any research on the topic of inflammatory conditions and dietary protein. The above article is one of several I found and the one I cite.
Remember, if you eat a 180 gram steak, you are not eating a 180 grams of protein! A beef eye fillet is about 22% protein, per CalorieKing.
Note for Older Australians
If you have a My Aged Care Plan you MAY be eligible to have your gym membership paid for through your plan. Your program would need to be developed by an exercise physiologist (verification requires paperwork!) or similar allied health professional.
In Closing
I hope this has been helpful. If you have any questions, drop them in the comments and I will respond.
If there is a topic you would like me to address, let me know!
Build that strength!