That was a long journey! But I am all good, the second knee replacement is done and shows every indication of being as great as the first knee replacement. July 26 was New Knee Day!
I wrote comprehensive articles relating to my first knee replacement. This time I’m writing about the differences between the two experiences.
The 2020 articles:
- My Total Knee Replacement (Knee Arthroplasty)
- Home: Now The Willpower Kicks In (Knee Arthroplasty)
- Thirteen Weeks! (Knee Arthroplasty)
I have NOW been told my 2020 recovery was “exceptional” while this recovery has been “typical”. They didn’t tell me that back in 2020, just that I was doing “so well”.
The Lead Up
As with the 2020 operation, this initial operation was also cancelled and rescheduled. In 2020 it was due to Covid-19 lockdowns. This time, in 2023, it was due to my psoriatic arthritis (PsA) being out of control. As well as medication for the PsA, I was also on NSAIDs and prednisolone as we (hopefully) waited for the medication to kick in. For surgery I had to reduce the NSAID dose from 400 mg p/d to ZERO. I had to get the prednisolone down to 2.5 mg p/d. I wrote about those requirements and what happened when I did a trial run in Crossing My Fingers – Again.
With the change to pain medication for me, my GP and I were confident we could handle the 10 days required with no NSAIDs, but yes, IT WAS DIFFICULT. By the time I was due to be admitted, I could barely use my hands at all before 11 am, as an example. The hospital admitted me the night before on medical grounds as there is no way I could have got myself there by 6:30 am the day of surgery.
I’ve talked about my teeth issues: yet another tooth (the third) played up just prior to surgery – in fact it split and half basically fell out in the dentist’s hand. My dentist advised it needs to be removed by an oral surgeon and did a temporary patch job. My GP had prescribed precautionary antibiotics which I arrived in hospital with. That caused quite a kerfuffle and there was talk of cancelling the surgery. Thankfully, that did not happen. My surgeon does not like surprises! Good thing too, but certainly was a bit traumatic at the time.
Last time neither my PsA or my teeth caused any complications!
Surgery
Pretty much the same as last time – I was out for it! However, surgeon came to me after surgery and said it was very “messy” once he got in there. The inflammation had caused damage to muscles that he could “stick his fingers into” (the holes). Will the muscles heal, I asked. He believed so. I forgot to ask which muscles! He last described it as “terrible”. I’m not sure if terrible is worse than messy!
Reading the letter the surgeon sent to my GP, it was again the popliteus muscle that was so badly damaged. This is the same muscle that was being dissected by a cyst in 2020, just this time it was worse.
The scar looks pretty much a mirror image of the left leg! it is also the same length – 23 cm for those into scar dimensions.
Post-Surgery
One good difference, one not so good.
First, the good difference. In 2020 my glutes spasmed uncontrollably and very painfully 10 hours after surgery. In the end, Lyrica was used to solve the problem. On that basis, the peri-operative physician decided to start me on Lyrica immediately post surgery. It worked, no spasms. My glutes, ITB and piriformis were still painful and needed physio work, but there was no crazy spasms like last time. Yay! I was also on far less pain medication overall with the change my GP and I had made and which the surgical team adhered to.
The not so good difference was my veins kept collapsing and we had to find new cannula sites. This was not fun, especially at 2 am in the morning. Why were they causing issues? I don’t really know, although having been on prednisolone for so long pre-surgery was suggested as a possibility. I ended up with quite a few bruises. The machine would beep madly and display “Downstream Occlusion”. I’ve left out the bruise photos!

The darn catheter was not a relief. I’d been rather looking forward to not having to worry about toilet trips immediately post surgery, but I felt as if I wanted to “go” all the time. Very annoying!
The x-rays look pretty much like last time! As does the dressing.



Of course I got makeup on and my nails done! The nails were done before the makeup and my hair is wet in the photo. But I was in hospital, so I’m allowed some leeway!


Rehab
Patient transport (to move me to the rehab hospital) was about 2.5 hours late and I nearly missed out on lunch!
Basically, rehab went pretty much like 2020. One difference was I left rehab still unable to do a straight leg raise. I managed to get those happening by four days later. It just took longer this time to get those quads really firing.
The other very sad difference was the wonderful massage therapist who had rooms at this hospital in 2020 is no longer there. Thankfully the physios treated my glutes and ITB!
The food was pretty good!



Home!
A hint. DO NOT accidentally hit your operated knee on anything. I did and I think I set myself back a week. Very grumpy with myself. I was a bit concerned and went to the surgeon’s office to have it checked on Monday (August 21). The nurse told me it looked fine, just to take it easy for a few days. So I did! Unusual for me, I know.
I’ve had ice packs on the knee and heat packs on my hands and glutes! Plus the spikey ball got a bit of use on the glutes too. Ice packs are good after the rehab exercises.
I am still taking pain medication, whereas in 2020 I had stopped by Day 20. As I write, this is Day 33 for this knee. I am older, the knee was messier and I accidentally hit it. Plus my PsA is still not under control (i.e. inflammation). My GP says to be realistic about the differences. I have reduced the pain meds considerably from when I first got home so that’s good.
I also have a theory about sleeping. My knee will be fine all day, but I’ll have pain or discomfort during the night. One night I woke up thrashing my leg around the bed, as if trying to shake off pain. Even this morning I woke up with the knee quite stiff. I think during our waking hours we are very careful and (usually) ensure we don’t do anything to hurt the knee. But when we sleep we toss and turn and can put the knee in positions it doesn’t actually like. We wake up as a result. Pain and/or stiffness can result. I wonder if bracing it at night might be a plan, but that only occurred to me today.
I am doing the rehab exercises religiously, as I did last time. On Friday (August 28) my flexion was measured at 128 and my extension was 100%! I never got to 100% extension with the left knee, I got to 98%. But I did get to 145 flexion at week 10, so that is again my aim. I may not get it, as I am heavier now than I was in 2020 due to the PsA and related meds this time around. It is still my target though.
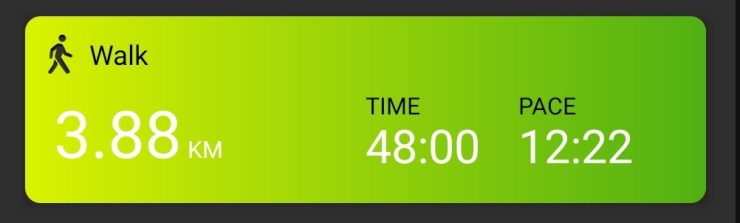
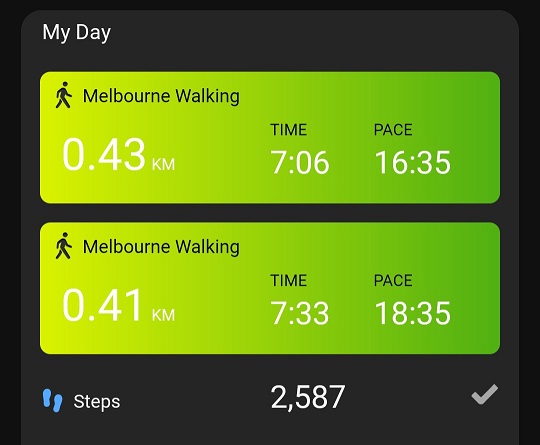
I am walking every day. Started with two little walks a day, gradually increased. Today I was back to my favourite walking spot!


Now, skip the next photo if you are squeamish. I think it looks great! Looks better now, this was a week ago. It is getting the Vit E treatment now. The scar from 2020 is barely visible any more.

So that about sums it up. As for the PsA, six days before surgery my rheumatologist changed my medication again, but I wasn’t allowed to start the new medication until 10 days after my surgery. It may take three months to know if this one works, so I am back on the NSAIDs and prednisolone while we wait. This is medication number 8. The hands are a little better now, but I am scared of counting my chickens before they hatch. The shoulders are also a little better. I do think I’ve been keeping Voltaren in business!
A Thank You!
Again, a very big THANK YOU to my surgical team. Same surgeon, same anaesthetist, same peri-operative physician as 2020. Absolutely fantastic. I am so happy to have matching knees!