This will be a series of articles! Too much information to cover in one.
Don’t worry, I am not trying to turn you all into Olympic Weight Lifters. I am definitely not an Olympic weight lifter, by any means! More and more studies are confirming that strength training is beneficial. And, believe it or not surprisingly good for people in their 90s. Both my general practitioner and my rheumatologist wholeheartedly support my efforts. To quote my general practitioner, “Strength training is so important”.
CAVEAT: This article assumes you have medical clearance to exercise. If you do not, please get clearance from your doctor. This article focuses on musculoskeletal chronic conditions but the underlying logic can be applied to many conditions.
I will admit to being biased. My fitness regime has always included weight lifting. That is not including lifting bales of hay and sheep on the farm! When I first became unwell, I had to take a break, but when I slowly started back, I wasn’t starting from scratch. I knew how to lift weights from past experience and I did a Fitness Coaching course specifically to learn more so I could keep myself as close to “healthy” as I could.
Practical experience taught me more aspects specific to having chronic conditions, musculoskeletal conditions in particular. When I did my qualifications, the course didn’t cover much about chronically ill clients. We did learn a bit about diabetic and asthmatic clients, but that was about it. From talking to other trainers who have qualified more recently than I, not a lot has changed in that respect. So bear in mind my advice in this article is based on my practical experience, building on what I learnt on the course. Think of your medical specialists – your rheumatologist did not graduate from medical school as a rheumatologist: a lot more study and experience and training was required. Personal trainers/fitness coaches are really no different. After they’ve completed their basic training they may go on to specialise in different aspects of training. Many will have such information about themselves publicly available on a web page. They may be like me, have medical conditions themselves and therefore have lived experience. They may have a family member or friend with a medical condition or just simply have an interest in the field and have undertaken additional training. Be prepared to interview your prospective trainers to ensure they have the appropriate experience to guide you. I will suggest some questions in Part II.
In my recent article, Accept the Project, I talked about the challenges we face when we initially find out we are now different. Generally our doctors will tell us to “get exercise” or “keep exercising” but it is not their role to give us specific instructions. As a result, many people will try to do what they did before. THAT IS NOT GOING TO WORK (unless you are extremely lucky). If you try to do that, the most likely outcome is you will end up in the Boom/Bust Cycle or, even worse, you may injure yourself.
My advice is start as if you’ve never picked up a dumbbell in your life before. If you have a history of weight training and are confident your technique is good, maybe you don’t need to consult a trainer. For complete novices, definitely consult a trainer. If you’ve had a considerable time away from lifting, I recommend consulting a trainer to ensure your technique is still correct. Technique (how you lift) is critical for healthy people, even more important for us.
Let me illustrate. If I am not in the perfect position when doing the shoulder press, my right shoulder will click. It doesn’t hurt, but I can feel it and hear it. It may not hurt now, but if I did that often enough, I’d very likely end up with an inflamed shoulder. My guess is my underlying conditions result in me not holding my shoulders in the correct position all the time, so I have to correct my posture before continuing with the set. But if we have no idea what correct technique for an exercise is, we could be doing it in a way that may exacerbate our situation rather than help us. I got caught the other day. I switched from tricep pushdowns to tricep kickbacks because my wrists didn’t like the pushdowns. One of the trainers pointed out my back was not in the correct position. Sometimes even when we KNOW how we should do something, because we can’t see ourselves, we don’t realise our technique needs correcting.
This next bit will be harder for some of us than for others. Sorry in advance! I used to do mostly free weights, not the machines. After I developed my condition(s), I realised quite quickly it is much safer to use the machines. Do I like using the machines instead of free weights? No. But I also know I need to be safe. Think of the chest press. If I am lying on a bench with a dumbbell in each hand and my body suddenly says, “No, sorry, not today” for whatever reason, I could lose control of those dumbbells and hurt myself in the process. On the chest press machine, at least the machine I use, I can transfer the load from my arms/hands to my feet very quickly (remember, I have bionic legs, so they cope!). In the picture below the foot rest can be seen. This moves as the handles move. Applying pressure to the footrest takes the load from the handles.

This way my chances of hurting myself are virtually zero. The machines can also be easier to adjust. Although we do aim to increase the weights over time just like any healthy person does, there will be days when for some unknown reason the body is just a bit “off”. I’ll put the pin in the plate I lifted two days prior and won’t be able to budge it. Very quick and easy to shift the pin to a lower weight without having to return dumbbells to the rack and get lighter ones. Usually dropping back by one plate is enough and I can keep going.
Having got those preparation aspects out of the way, what weights and exercises should you start with? You know what my answer is before I even type it, don’t you? IT DEPENDS! On so many things. Below is an example of what I am currently doing. This will be way too much for some people and others will scoff at my (to them) meagre weights. Yes, this is also an issue for those with a past history of lifting. I used to leg press over 200 kgs. My personal best since developing chronic conditions is 160 kg. At the moment I am sitting on 125 kg. If you are a competitive person it can be VERY, VERY hard to accept you are very unlikely to lift your previous weights again. My bicep curls are currently 12 kg – 2 x 6 kg dumbbells. Nothing wrong with my biceps, but prior to my recent new diagnosis my wrists couldn’t cope with anything heavier than about 4 kg. In my forties I was using much heavier weights. This is something we have to accept. We are now different, we have to have different goals.
THIS IS NOT WHERE YOU START! I’m merely illustrating what is possible over time.
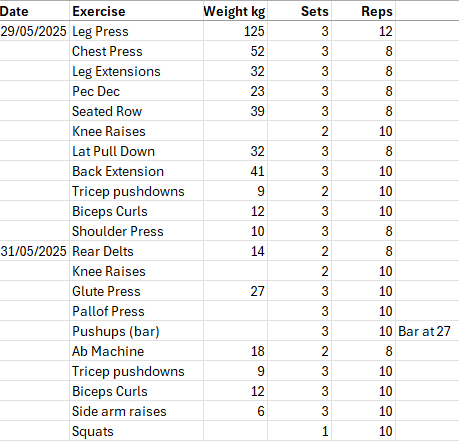
The above shows two days. I go to the gym three days a week: Thursday, Saturday and Monday. The Thursday and Monday are fairly similar, but the Saturday is a lighter day and I do different exercises than the other two days. At the moment: I can change things around at any time.
Why are some sets only 8 reps and other 12? Usually 8 will indicate I’ve just increased the weight, 12 will indicate I am about to increase the weight. On the other hand, a 12 may indicate I have dropped a weight because that body part is not as happy as usual and I’m waiting for it to settle, so I’ve dropped the weight and increased the reps.
No, there isn’t a lot of core in that list. A lot of core exercises are on the floor and those I do at home. I also have a swiss ball at home. I don’t usually do squats at the gym, but that particular day I was short on total time so threw a set in to reach my time target.
In Part II of this series I discuss how you determine where to start on this journey. What questions might you ask a prospective trainer? What might be a good program? How many times a week? What kilograms might you start with?
Further Reading:
Not everything in the articles below is applicable to those with chronic conditions, but clearly the benefits of strength training are being recognised.
The ninetysomethings who revolutionized how we think about strength training – The Guardian
From strength training in your 20s to yoga in your 80s: how to reach peak fitness at any age – The Guardian
‘Never think you’re too old’: meet the world’s fastest 75-year-old woman – The Guardian
















