I’ll start this article with clarification. This article will not apply to every person (remember we are all different) or every chronic illness or disease. But it does apply to many of us in the chronic illness population demographic. Remember, at least 47% of the population have at least one of just ten nominated chronic illnesses, so there are a few of us.
Please note as you read, I am using the word “accept” as per this Thesaurus definition: to accept or continue in a situation that is difficult or unpleasant: accept can be used when you want to say that you know a difficult situation will not change and you have decided to stop trying to change it.
But you CAN manage it in many cases. With, of course, the expertise of your doctors and allied health practitioners (physiotherapy, osteopathy, myotherapy, exercise physiologists particularly). Manage it to the point it is far less unpleasant.
The very first thing we have to do is truly accept the new us. Like you accept a new project in the work environment. Now, you may not like that project, you may not want to undertake that project: but you need to feed and clothe yourself, so you accept the project. You take it on board. You embrace it and do it to the best of your ability.
Discovering you have a chronic illness is a shock, no doubt about it. Many of us initially do some or all of the following:
- Hope it will go away
- Hope the medicine will do all the hard work
- Deny the reality of the illness
- Try to keep living “normally”, ignoring the illness
- Think if they change aspects of their life to accommodate the illness they are “giving up”
The last one is the big one here. Let’s go back to the project at work analogy. To take on that project you may have to delegate some of your current role to other staff. You may need to relocate your office. You may have to hire new staff. Any number of aspects of your current work may have to change. You will have to set project milestones and goals.
With a chronic illness, same deal. YOU are the Project Manager of your life. To all intents and purposes, your doctors are your new employees (sorry, doctors, don’t read that the wrong way!).
It takes time to accept this new role. I estimate it took me four years. Oh, I started the Movement As Medicine immediately: it was the other things that took longer. Like cutting my work hours to part-time. Eventually I retired earlier than I would have liked. I’ve spoken to other patients who cite times from one and a half years to eight years. The risk of not accepting this new Project is that your illness may progress faster (or quite simply drain you) than it otherwise would have.
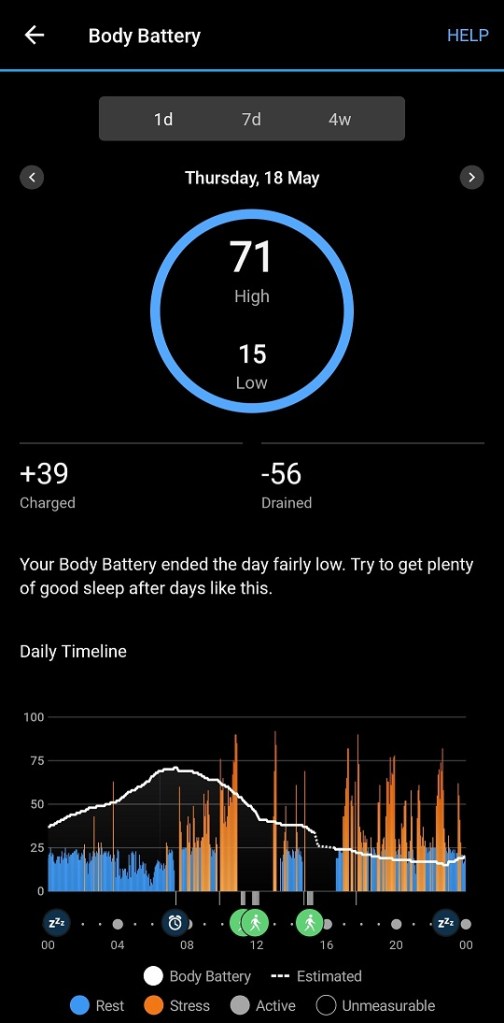
As I have written in the past, the energy depletion with many chronic illnesses can be astounding. If, for example, we continue to work full-time, at the end of the day we are exhausted. No Movement As Medicine happens. Weekends are spent recovering some energy for the next week. Or if we see getting My Aged Care as “giving in”, we are using our energy reserves to do housework rather than care for our bodies.
I have a damaged lumbar spine (result of a car accident about 44 years ago). In 2016 surgery was considered, as the pain was consistent and rather debilitating. That surgery would not have been permanent. Instead, I elected to try strengthening my posterior chain. It is now 2025 and that has been successful – no radiofrequency denervation of the lumbar spine for me! While not directly part of my illness, my illness (as do many illnesses) does love to exacerbate weak spots – a 44 year-old injury is a weak spot.
Clearly, to work on my posterior chain strength I need both time AND energy. Project Management priorities! Should I have continued working full-time and hoped my back would right itself? We all know that would have been unlikely. Or dropped my working hours and used that energy and time to work on my body?
If you are diagnosed with a chronic illness, you cannot ignore it in the hope it will go away. This IS the new you. The faster you take on that Project Manager role, the better your chances of maintaining your independence, mobility and freedom for as long as possible will be.
Stavros is another patient who took on the Project Manager role. You can read his Type 2 Diabetes story here: https://dodona777.com/2025/05/16/why-dont-people-choose-to-heal/ Stavros took charge of his project: control his Type 2 Diabetes.
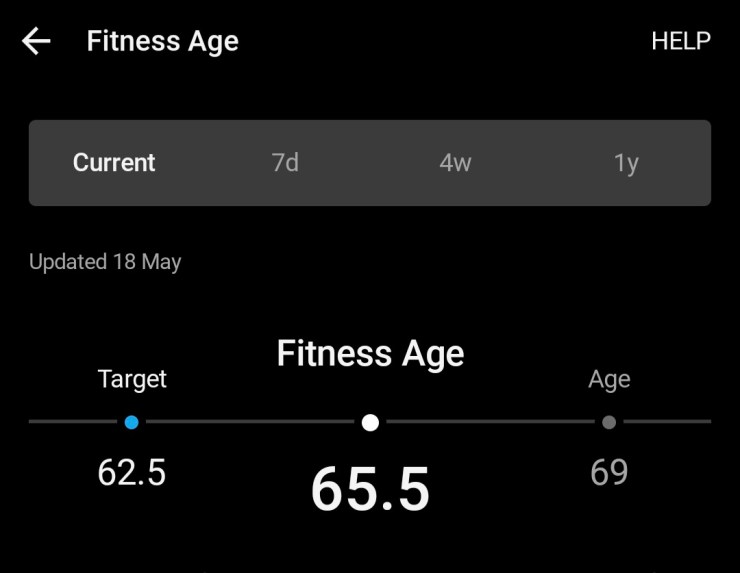
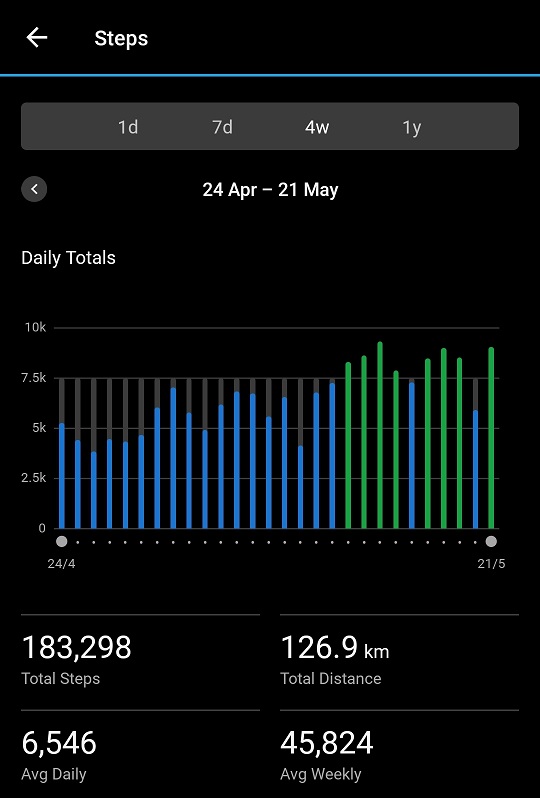
Yes, I know I’ve been quiet for months! You see, I’ve been so wrapped up in enjoying my much improved body since the new diagnosis, and getting my own Movement As Medicine back on track, that’s been my primary focus (evidenced by the feature photo). I’ve increased my weight lifting/training from every third day to three times a week. For any readers raising their eyebrows about strength training, in closing I refer you to recent research findings:
The residents’ average age was 88, and three-quarters of them were women. Every resident had multiple medical conditions. Almost half required help to engage in the essential activities of daily life: getting out of bed, going to the bathroom, bathing, walking, eating.
One simple exercise proved older adults can build and retain muscle – and caused a paradigm shift in science
Source: The Guardian The ninetysomethings who revolutionized how we think about strength training