When those of us with chronic conditions get something else, as I recently did, our situation can become a little more complicated. The journey back to where we were before this something else disrupted our routine can be challenging. Moreso the less young we are, sadly. Par for the course for many in the over 50 demographic, not just the chronic illness community. We decondition faster the less young we are.
So what happened? I started getting a slight temperature, then it became a fever. It would go up and down. Given my clinical status as a “complex comorbid chronically ill person”, I thought it would be wise to alert my GP (general practitioner) to the situation. My GP was fully booked but organised for a colleague to see me. The colleague ran a host of tests, including blood cultures! I’d never had blood cultures before. Funny story – as the phlebotomist was drawing blood, I noticed the expiry date on two of the four blood culture bottles was past. So I had to give an extra one! Spotted before the second expired one was taken.
By the Friday August 8 my temp was higher. Messaged GP clinic. Advised to go to hospital. So I did. Was not expecting to be admitted, so hadn’t even taken a toothbrush with me! Consequently I begged them to allow me to go home and come back the next day. Properly equipped for being an inpatient.
After more MRIs, CTs, x-rays, blood tests and blood cultures that you can poke a stick at, I was finally discharged on August 13. If you’ve never seen a blood culture bottle, they look like this! And seem to come in pairs.

My diagnosis? Atypical pneumonia. Hard to diagnose, but the antibiotics prescribed did the job. One lung lobe looked “flat” on imaging and they could hear a rattle in the other lobe. But a fluctuating fever and chills were the only real symptoms I had: no coughing or headaches. I had been experiencing intermittent pain under my left rib (mostly in the evenings) for a few weeks. Related? I don’t know, but it seems to have stopped since the antibiotics.
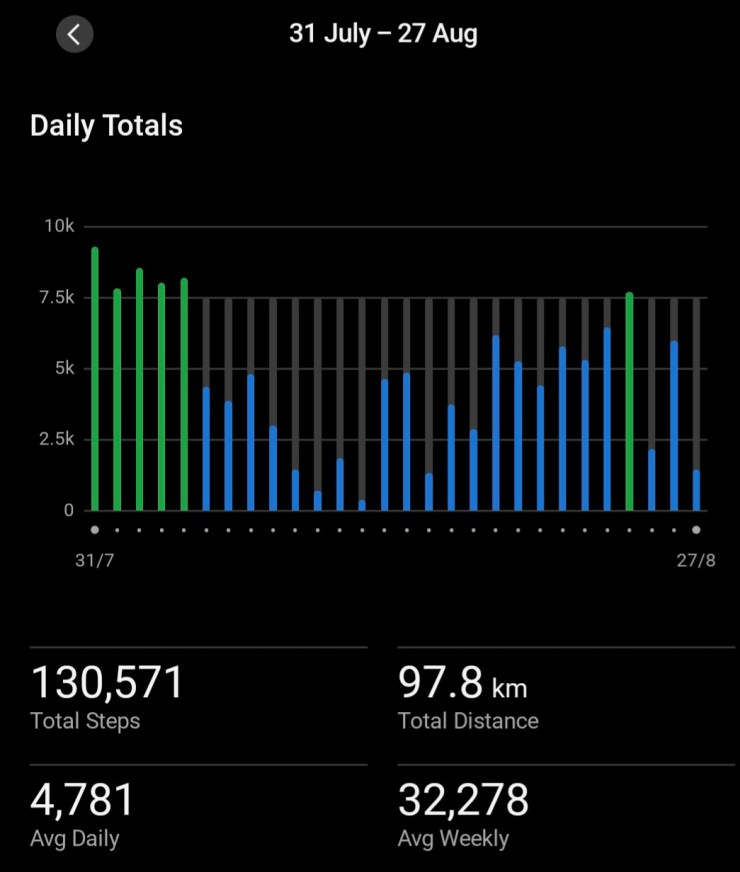
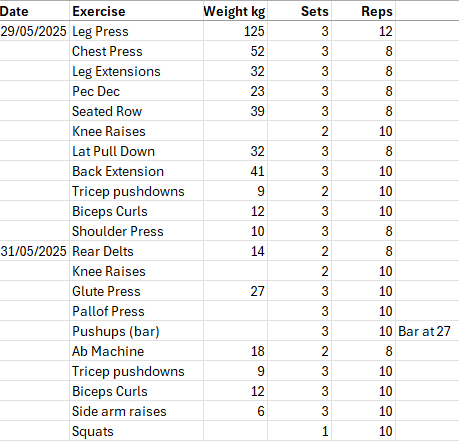
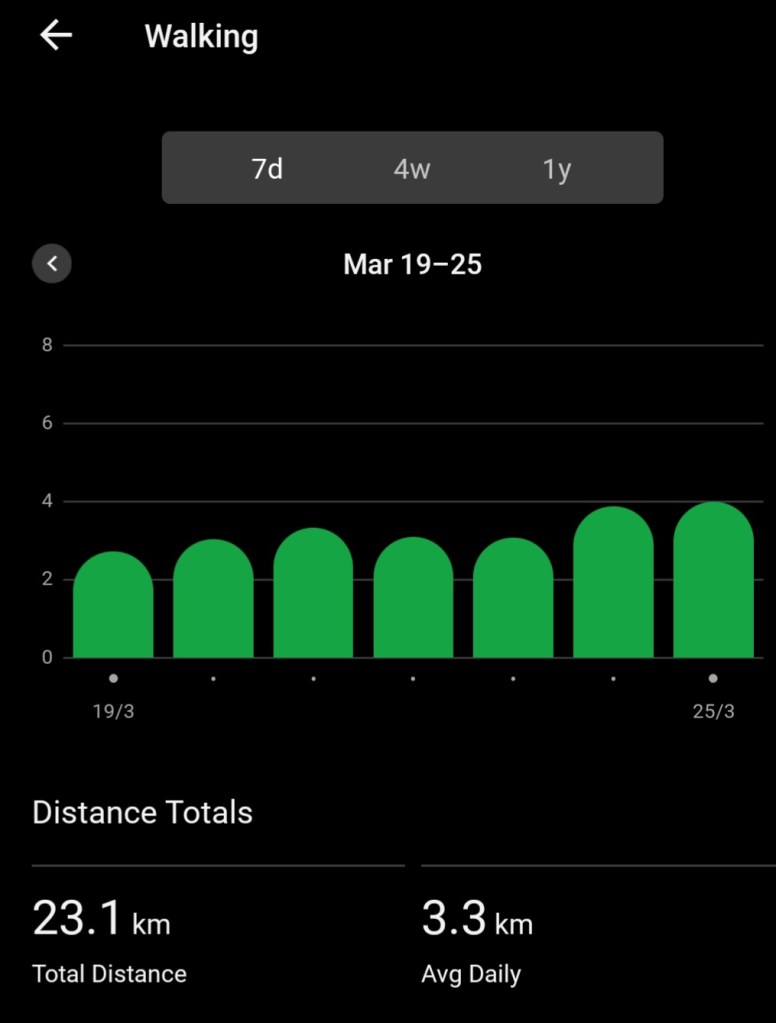
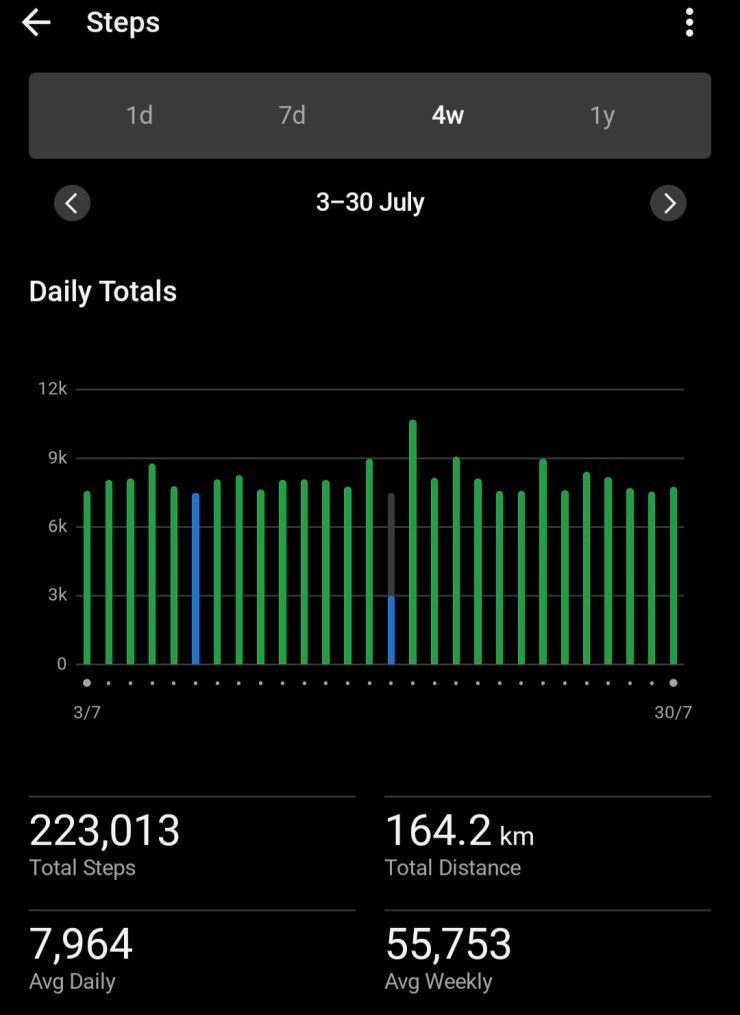
Due to this event, my exercise regime had just stopped. I’d last been to the gym on August 2, finally got back on August 18. So a 16 day break, not just in strength training but also walking/step goal. Above is the graph of steps I have achieved this last four weeks. July is shown below for comparison. Big difference.
My lumbar spine is still complaining as I’ve lost muscle tone in my posterior chain, but I am seeing gradual improvement. HOWEVER many of my metrics are still showing a loss of fitness and strength:
- My resting heart rate has increased by 8 points
- My walking speed has dropped
- My vigorous intensity minutes per day goal is not attainable at the moment
- I’ve had to drop my weights for several exercises
For example, I was at the gym yesterday. My usual practice is to walk 500 metres on the treadmill as a warm-up. I was breathing quite hard at 4.8 kms per hour. NOT my usual by any means. Garmin told me it would take me seven hours to recover. Normally Garmin tells me 0 hours (yes, zero, that’s not a typo) for 500 metres at a speed of 5.5 kms per hour. I’d had to drop my chest press from from 59 kg to 39 kg – got back to 52 kg yesterday.
Even lifting weights yesterday caused me to breath harder than I usually do. I’m seeing my GP next week to confirm, but have read it can take six weeks to fully recover lung capacity. I’m pretty sure I don’t need any pulmonary rehabilitation, I just need to build back up at a sensible rate. I must not overdo it!
Of course, me being me, not rushing things is not easy. I want to be back where I was before all this happened. The hospital experience was a little confusing too. One doctor told me I couldn’t take Panadol Osteo, just Panadol for my back. Another told me to stop one of my arthritis medications, the next day another doctor told me I could take that medication. All of this was because they weren’t quite sure what was wrong with me. At one stage I wasn’t allowed out of my room and there was a big sign on my door that staff entering had to take precautions.
Given my experience since I’ve been home, that is what I can only describe as reduced lung capacity, I’m pretty sure the doctor diagnosing me got it right. Even so, I had to agree to try the antibiotics as the diagnosis wasn’t one of those ones where you have a blood test and there is a clear positive or negative result!
Getting back to where I was before all this will take time and I must not rush it. So that is my advice to anyone else who finds themselves in my position – where we suddenly get something else and that throws a spanner in the works. Be careful. Don’t not do anything (unless there is medical advice due to your specific condition) because that will lead to other aspects (like my back) deteriorating. On the other hand, we can’t go overboard and try to rush things either.
I’m not sure how long it will take me to get back to where I was in July, I’m hoping just a few weeks. I think I was relatively fortunate as I didn’t end up with a severe case of pneumonia. Maybe partly because I got onto it quickly and my GP took action. If anything seems amiss, see your doctor!