Thankfully, my second knee replacement surgery is back on the agenda! Woo hoo! I’m excited!
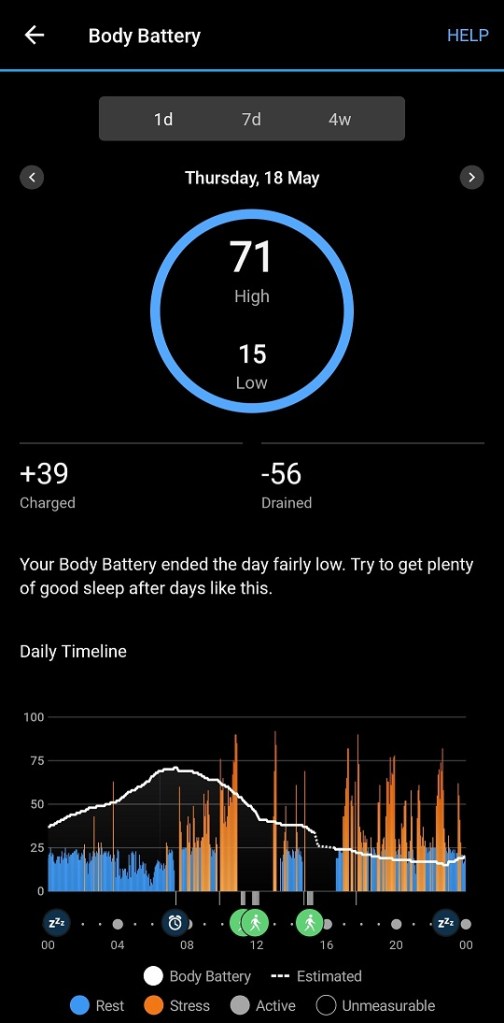
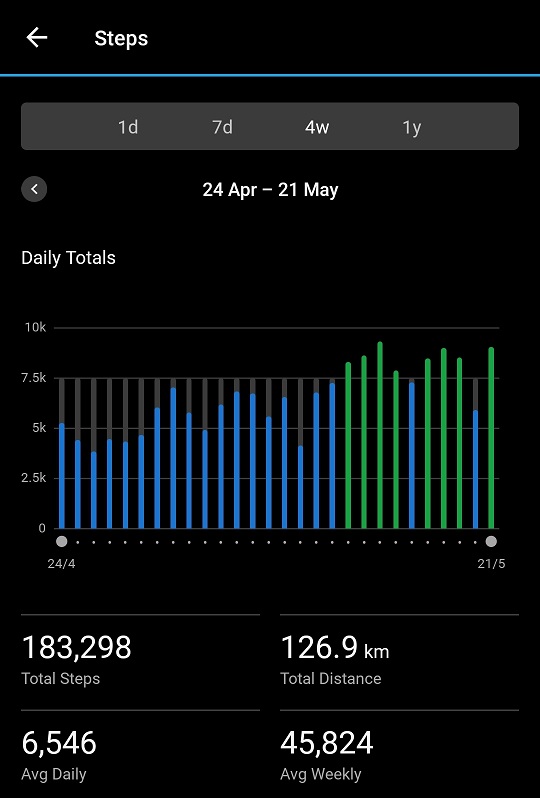
I suspect some people may wonder why I am getting a knee replaced if I can walk 7,500 to 8,000 steps a day and do “formal” walks totaling 4 kilometres a day. How can my knee be THAT bad if I can do that? Only due to great care and diligence, let me tell you. The aim of this article is to give some tips on how to manage walking leading up to surgery. If I don’t replace the knee, I am very limited in what I can do. I can’t spend my life walking in a straight line.
As described in Crossing my Fingers – Again, we felt my new biologic was finally kicking in. My GP wanted me to keep my medication dosages stable for a week or two, which we did. On May 30 I dropped my NSAID dose by half and have managed to maintain that. I saw my GP again on June 6. We felt if I got a surgery date, we’d make it. So I have a date! Next month! Now, we recognise that during the 10 days before surgery where I have to be at zero NSAIDs, I MAY have to increase my pain medication to compensate, but as this is only for 10 days, that’s acceptable. I did something similar for the last knee surgery too (there are links at the bottom of that article to the full knee replacement story). I also have to reduce my prednisolone, which I have starting doing this week. I’m NOT pain free, by any means, but I’m surviving!
I do have to be very careful to keep the bung knee in line, no twisting! I can’t fully extend it, although flexion is not quite as bad. Bending down to pick something up off the floor? OUCH! Having it bent while sitting at a dining table, for example, results in pain when I first get up from the chair.
I need to keep exercising to ensure I’m ready for rehab. Last time I was doing glute bridges on the dining table. Sadly, down I’ve downsized, my dining table is doubling as a desk, so I have to find other ways.
Here are my walking tips.
- Make sure you have good, supportive shoes. This is an absolute must.
- Choose a pleasant place to walk if you can. The photo above is where I love to walk. It is encouraging!
- Keep an eye on the terrain. If I accidentally step into a small pothole with my bad leg, the pain is NOT GOOD.
- Pay attention to your posture. If walking in a shopping strip, shop windows can be useful. In a park, check your shadow. Is your back straight? Shoulders back?
- You may start limping because your body may decide to shorten your stride on the bad leg without you even thinking about it. Try to maintain the stride length if the pain is not too bad. This will depend on several things: what pain management program you have going, how bad the joint is, etc. You will need to “warm up” first, but I find I can control the limping without increasing the pain. Why is this important? Because you don’t want to shorten and/or tighten soft tissue like tendons prior to surgery if you can avoid it.
- Down with the bad, up with the good. When negotiating steps, stairs or gutters on pavements etc, down with the bad leg, up with the good leg. Why? Less bending of the bad leg (especially bad knees). I stupidly walked down the stairs to the car park in a hospital the other day. Very bad decision, I should have waited for the lift! Even with this tip, stairs are hard to negotiate!
- Inclines and declines. Where I walk there are very slight (well, very slight for MOST people) inclines and declines. Some on the actual path, but also bridges like this. While I have little problem with the incline, the decline is difficult. Depending on where the damage is in your knee (or other joint) you may find the reverse, or you may find both are a little challenging. Slow down, hold the rails if there are some, maybe decide that track is not for you in future.

- Don’t walk until you’ve “thawed out”. As we know, psoriatic arthritis is notoriously bad in the mornings. I take time in the morning to gently thaw myself out. The knee awaiting surgery will most likely also stiffen up overnight. While some mornings are better than others, I rarely do my first walk of the day before 10 am, sometimes not until 11 am. Even then, the first 200 metres or so are warming up.
- Split the walking if at all possible. I’m retired, I can walk whenever I like, but obviously some patients are still employed. If you can break up the walking, do. At the moment it takes me about 15 minutes to walk a kilometre. You can fit a kilometre in here or there throughout the day. Take a slightly shorter lunch and a longer tea break, perhaps. Not possible in all jobs, I know. Winter means walking after work is not really appealing. Think about ways you can split the load.
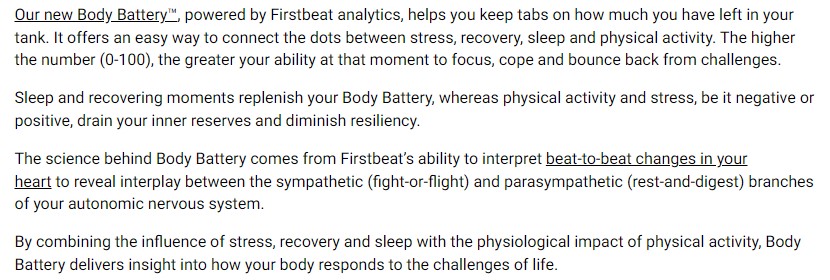
- As we all have different pain management regimes, I can only speak of mine. At the moment I am on a slow release (SR) twice a day and have some instant release (IR) for breakthrough pain. On a day where I’m not too bad, I may need no IR at all. If I am feeling the knee is a little too grumpy, I’ll time the taking of an IR (maybe only half) so that it kicks in before I start walking. This is all about listening to your body.
- When you get home from a walk, I suggest elevating your feet for a while, but do not allow your legs to “freeze up”.
- Remember to adjust your goals if you are doing other “stuff”, as I discuss in Why is There a Dip in My Stats?.
Once I have done the first walk of the day, I usually have very low pain levels for the rest of the day. We are all different, our joint damage is different and some, like me, have underlying conditions such as psoriatic which do complicate matters. So while that is my situation, I accept it may not be yours.
I also have two ankles requiring surgery. The left ankle is very problematic at the moment. When I was on my higher dose of NSAID I would know when I hit 500 metres on my first walk of the day as all of a sudden, the ankle would stop hurting as much. When I dropped the NSAID dose on May 30, from then it has taken about 800 metres before my ankle stops hurting. Hence it is important I time that IR dose properly if I feel it necessary. When I say “stop hurting” do I mean pain free? No, sadly, I don’t. Some days are better than others, but the level of pain is low enough that I can keep up the walking. And, once it is gone, it is pretty much gone for the rest of the day, thankfully.
We are all different. Please talk to your doctor and/or physio about what may be specifically appropriate for you.
Do not expect every day to be the same. For some weird reason this morning was awful for me. I even battled to pull my sheets out of the washing machine (nothing to do with my knee). I had a nanna nap after lunch (VERY unusual for me). Yet now, as I write, I am fine. I reduced my prednisolone yesterday morning, I think my body is adjusting to that reduction.
If you have any questions, I am always here to help if I can.
Addendum: The following is a good article from The Guardian about walking technique.