I sent the email below to VicRoads on Monday March 7, 2022. As of today, I have not received a response. Some patient experience in the meantime. On Saturday I went to the gym. The closest park I could get was 300 metres from the gym. This was a suburban gym, not a large shopping centre as cited in the email below. That meant I had to cut my rehab work time short to allow for the extra energy required to walk an unplanned extra 600 metres (total). On the Sunday I went to the same location for hydrotherapy. Hydrotherapy means I am lugging an equipment bag and a swim bag. I knew if I was going to have to park as far away again, I would have to skip my hydrotherapy. Thankfully, I was able to get a park across the road. Even so, once I had finished my workout I had to sit and rest for ten minutes before walking back to my car. Energy.
I believe a week is sufficient time to allow for a response. When I do receive a response, I will do a follow-up article. This issue is going to be very important for many chronically ill people.
Dear VicRoads,
I recently renewed my accessible parking permit. This is the first time I have been through the VicRoads application/renewal process as in 2021 I renewed via City of Stonnington.
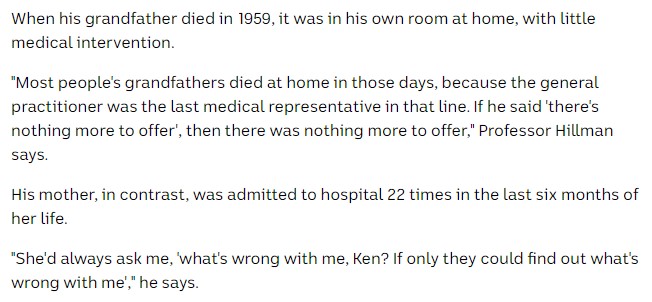
I had a total knee replacement in 2020 and bi-lateral foot surgery in 2021. Those are not the reasons for my concern. My concern relates to my chronic condition, psoriatic arthritis. As with many chronic conditions lethargy and fatigue are symptoms. A DT Permit is of very little benefit to me and the many patients like me. I hope that the decision makers and policy makers within VicRoads are aware of the prevalence of lethargy and fatigue. If not, there are many peer reviewed clinical reports I can refer to your organisation for their edification.
You may have heard of the spoon theory analogy. Personally I prefer the internal battery analogy. Most chronic illness patients have limited battery charge per day. I refer you to my own writing, “Personal Energy Use” for a deeper explanation.
The DT Permit provides no proximity benefit to the permit holder. For example, in a large shopping centre or university carpark I might have to walk a kilometre just to access the shops or lecture theatres and return to my car. That doesn’t take into account any walking required within the shopping centre or on the campus. Large hospitals could require similar. I know, because I’ve measured the distances.
For a person with a chronic condition, this extra energy use may prevent us being able to shop, receive health care or undertake education. Alternatively, it may leave us so depleted of energy we are unable to undertake the activities that are required to manage our condition on a daily basis or to perform our jobs effectively. I currently work from home, however when required to go into the office, in a very large organisation, getting a car park near a lift can be extremely challenging unless I have an ADP Permit.
Surely it would not be difficult to mark some standard width carparks within a reasonable proximity to appropriate entrances to the facilities in question.
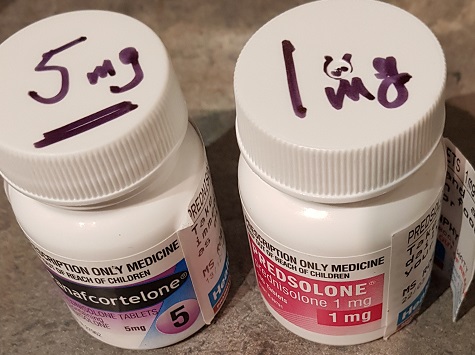
The DT Permits do not allow for changing circumstances either. For example, psoriatic arthritis is notoriously unpredictable. While I’m not using any mobility aids at the moment due to a recent change in medication, two months ago I couldn’t get out of bed without using crutches. I am facing a second total knee replacement and two ankle replacement surgeries in the future. The ankle replacements require twelve weeks each of non-weight bearing on the operated leg (a knee scooter allows mobility). Obviously while on a knee scooter I will require one of the wider car spaces (no, I will not be driving myself). I understand temporary ADP Permits can be obtained for surgical reasons, yet this does not change the underlying issues of the DT Permits nor allow for unpredictable conditions.
The VicRoads website restricts the ADP Permit to issues with walking less than 100 metres: “you have an acute or chronic medical condition such that minimal walking (up to 100 metres) causes you to stop several times because of pain, extreme fatigue or imbalance which may endanger your health acutely in the long term“.
This is unrealistic for the reasons I have stated above. It isn’t the 100 metres that will be the issue for many of us, it is the energy expended walking the considerable distances given there is no proximity benefit with an DT Permit that may cause extreme fatigue which may endanger our health in the long term and impact our current quality of life in other ways as stated above.
I hope that VicRoads will give serious consideration to the requirements. My permits (expired and current) are attached for your reference.
I will be publishing this letter on my website in order to support the disability community but will await your response.
Kind regards
Addendum: For those wondering, yes, there are differences between states. There is an Australian Disability Parking Scheme, details of which can be found on that link. Note that the DT permit is NOT part of the federal scheme and therefore is not accepted in other states.
Update March 26, 2022 Please refer to Accessible Parking Permits – Part II for an update.